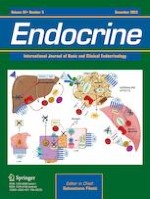
Fig. 1
Suggested effects of adrenaline in glucose metabolism. Cross-talk among muscle, adipose tissue, liver, pancreas and gut. In skeletal muscle, beta 2 adrenergic receptor (β2) stimulation increases glucose transporter 4 (GLUT-4) translocation to plasma membrane and glucose (GLU) uptake, via mammalian target of rapamycin complex 2 (mTORC2) and cyclic adenosine monophosphate (cAMP) signaling. The intrinsic activity of GLUT-4 is enhanced in the absence of insulin (INS) and inhibited in the presence of INS. Intracellularly, metabolism is shifted to glycogenolysis and aerobic glycolysis, leading to increased release of lactate (Lac) and alanine (Ala) in the bloodstream. In adipose tissue, beta 3 adrenergic receptor (β3), stimulates lipolysis and free fatty acid (FFA) release in the bloodstream. In turn, lipolytic products induce mTOR complex 1 and 2 (mTORC1-2) dissociation, leading to inhibition of phosphatidylinositol-3 kinase (PI3K) - protein kinase B (Akt) - mTOR pathway and, therefore to decreased insulin-mediated GLUT-4 translocation and GLU uptake. In parallel, β3 affects basal GLU uptake via cAMP signaling, in biphasic mode, depending on adrenaline (A) level. At low A level, the intrinsic activity of GLUT-4 is promoted leading to enhanced GLU uptake, while at high level, GLU uptake is compromised. Meanwhile, downregulation of adiponectin (ADIP), upregulation of resistin (RES) and inflammation further exacerbate insulin resistance. In liver, increased influx of gluconeogenesis substrates, i.e. Lac, Ala and FFA, together with inhibition of glucose uptake by glucose transporter 2 (GLUT-2) and β2-induced expression of phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phophatase (G6P) enhance gluconeogenesis, in parallel with increasing glucogenolysis. These effects are further exacerbated by augmented glucagon (GLUC) secretion. The secretion of the latter from alpha pancreatic cells, is upregulated upon β2 stimulation, via cAMP-induced activation of protein kinase A (PKA) and exchange protein directly activated by cAMP (EPAC2), which, in turn, activate two-pore channel 2 (Tpcn2), resulting into increased intracellular calcium (Ca2+) and exocytosis of GLUC granules. In beta cells, alpha 2 subtype alpha adrenergic receptor (α2α) induces membrane repolarisation or inhibition of voltage-dependent calcium channels, leading to decreased intracellular Ca2+. Additionally, α2α attenuate the glucose-induced and glucagon-like peptide 1(GLP-1) potentiated cAMP production, leading to inhibition of transient receptor potential melastatin 2 (TRPM2) and decreased beta cell membrane excitability. Finally, α2α inhibits GLP-1 production from L-enteroendocrine cells (L-cells). All these phenomena synergistically decrease INS secretion. A-responsive genes are represented by parallelograms, colored light blue if upregulated and brown if downregulated. Intracellular proteins are represented by light green oval shape and cAMP by beige oval shape. Adrenergic receptors are displayed by G-protein coupled receptor transmembrane structure and ion channels are depicted in both closed and open forms, according to the occurring effect. GLU is represented by red oval shape, Lac by ocher oval shape, Ala by fuchsia oval shape, FFA by yellow star-like shape, INS by light blue triangle, GLUC by purple trapezium, and GLP-1 by beige parallelograms. The occurring stimulatory or inhibitory effects are represented by solid arrow (red color) and inhibitor lines (black color); the latter are also demonstrated by black crosses. Dashed arrow lines are used to describe ambiguity of GLUT-4 function, according to its intrinsic activity. A adrenaline, Akt protein kinase B, Ala alanine, ADIP adiponectin, Ca2+ calcium/calcium channel, cAMP cyclic adenosine monophosphate, EPAC2 exchange protein directly activated by cAMP, FFA free fatty acid, GLP-1 glucagon-like peptide 1, G6P glucose-6 phosphatase, GLU glucose, GLUC glucagon, GLUT-2 glucose transporter 2, GLUT-4 glucose transporter 4, INS insulin, K+ potassium channel, Lac lactate, L cell L enteroendocrine cell, mTORC1-2 mammalian target of rapamycin complex 1-2, mTORC2 mammalian target of rapamycin complex 2, PEPCK phosphoenolpyruvate carboxykinase, PI3K phosphatidylinositol 3-kinase, PKA protein kinase A, TRPM2 transient receptor potential melastatin 2 channel, Tpcn2 two-pore channel 2, α2α alpha 2α adrenergic receptor, α cell alpha pancreatic cell, β2 beta 2 adrenergic receptor, β3 beta 3 adrenergic receptor, β cell beta pancreatic cell